There is something called "oversupply" or "hyperlactation" or "overactive milk ejection" that can be a mixed blessing. You sure get to store up a bunch of milk if you are pumping but if you don't remove the milk adequately, you can get recurrent plugged ducts and mastitis.
We don't know really why it happens. The ability to produce breastmilk exists on a spectrum. On one end, we have moms who aren't able to produce enough milk. I can usually help with that, or at least attempt to explain it. On the opposite side of the spectrum are the moms who can't ever seem to be empty, leaking through clothes and bedding, pumping crazy amounts of milk even when their obviously -full baby is done eating.
Signs of oversupply and fast flow that get mistaken for something else:
These babies can be very irritable, which can be interpreted as colic or reflux. Many of these babies are placed on medications for reflux. Reflux is a symptom, and the medications used to treat it are consistently shown in studies to be ineffective with potentially dangerous side effects. Often the irritability is treated with a maternal food elimination diet which is unlikely to be beneficial unless the oversupply has gone unnoticed for a while and the baby is now having gut complications. These babies have a tendency to sound congested. While the nasal airway is protected from food that is headed into the gut, it is not protected from very fast flow or from food headed up from the gut. The congestion is likely food, not infection. These babies feed frequently, gain weight very quickly, are often “colicky” and have explosive watery bowel movements. Mothers of these children are often told to wean the baby since the child is “allergic” to the milk. Breastmilk allergy is extremely rare if it even occurs.
Overabundance of maternal milk should be distinguished from other reasons for breast fullness, such as engorgement, which may be related to a poor latch and poor milk transfer from the breast. These babies should be managed with the help of someone experienced in assessing breastfeeding complications.
Orally defensive behaviors that get mistaken for something else
Babies who are dealing with fast flow will often develop ways to protect themselves from that noxious stimulation. They may bite and pull back on the nipple during a milk ejection reflex (let down) causing nipple pain and redness that is mistaken for nipple yeast. They may cry after suckling for a few minutes, or during the middle of a feeding, which may trigger a diagnosis of reflux but when the baby has only been on the breast for two minutes, what's to reflux? They are responding to the first let down. They may cry with each let down if it is forceful.
The significance of choking and sputtering
Babies who are choking and sputtering are dealing with breastmilk near the airway. These babies can get so much milk there that they struggle to breathe and are at risk for aspriation. We need to urgently address these babies.
Position first.
These babies need to be fed in a way which works with their physiology: prone, on mother's chest, and given the chance to self-attach. Too often, these babies are in a cross-cradle or cradle hold which places the baby essentially supine with the milk flowing down into their throat and with the aid of gravity. We need to stop using these positions with newborns. Babies can latch by themselves and it is especially important for these babies so that they pick how much breast tissue they will take in, allowing them to control the flow. In a position where the baby is prone on mom's reclined body, the baby is coming at the breast from the top, with baby in control of the flow, because we are working against gravity.
A baby dealing with fast flow will often be gassy and always hungry. This is due to varying degrees of fat during the feeding. (We called this foremilk and hindmilk at one time which lead to confusion and overthinking.) The amount of lactose is consistent across a feeding but fat is not, gradually increasing throughout the feeding. The hormones of satiety are found in the fat component of milk. The more milk removed, the higher the fat content, the more hormones of satiety. A baby fed supine gulped the meal, getting little fat. A low fat diet causes the stomach to empty faster. As a result, the enzyme lactase, which breaks down the breastmilk sugar lactose, isn't made in high enough quantities and some of that lactose goes undigested. This leads to a lactose overload causing gas and explosive stools. Most moms (and their providers) blame something in their diet. This is not lactose intolerance, which is extremely rare in infancy.
We need to get more fat in the milk. One way is to change position and slow down the flow as we discussed. The amount of fat slowly increases over a feeding, releasing a gut hormone called cholecystokinin (CCK) and CCK is one hormone that tells your brain you are full. It also acts on opiod receptors and is responsible for that floppy, contented look babies get after a good feeding. We can borrow what we know from the research on hands-on pumping and breast massage to increase the fat in pumped milk for babies in the NICU.
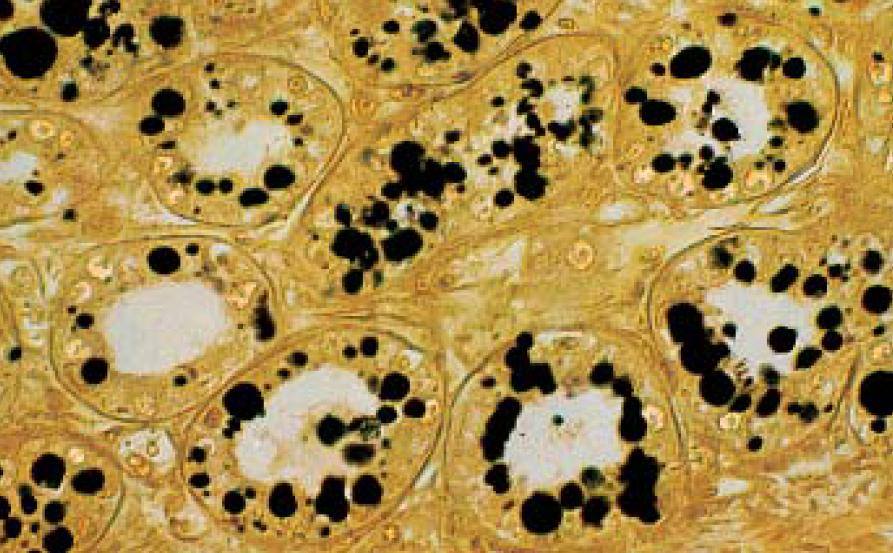
The picture shows fat cells stained black. They stick to the cells of the alveoli and don't enter milk until the alveoli starts to shrink from decreasing milk content. Hand-on pumping, massage with hands (or as some of us like to use, a vibrating kids toothbrush) can loosen the grip those fat cells have and send them into the at earlier, increasing fat content.
So, position first, then use strategies to increase fat in the milk. If that doesn't help, a nipple shield may help. Here's what it looks like (and I have them in the office) You can see that it might serve as a "breakwater" to slow things down a bit. We could also use drugs, although this is a desperate measure. For example, while pseudoephedrine is compatible with breastfeeding, just one 60 mg capsule can suppress milk production. You should only take that much medication after speaking to your physician since increased amounts of pseudoephedrine can cause elevations in heart rate, blood pressure and anxiety.
We don't necessarily have to fix the oversupply (we absolutely do if the baby is choking and sputtering!). Not every infant as symptoms due to fast flow. Increased amounts of milk may come in handy for later use, such as a return to the workplace. We could also consider donating it to our local milk bank, the Mother's Milk Bank of the Western Great Lakes.