Too many women are told to discard their milk because of the need
for medication. Often, this information is just plain wrong, causing unnecessary interruptions of breastfeeding, impacting milk supply and
confidence, and creating unneeded expenses.
Breastmilk is protected from blood by a a blood:milk barrier very similar to the
blood:brain barrier. In order for a
medication to cross from the bloodstream into breastmilk it has to be able to
cross that blood:milk barrier.![]() <---
I have cool
slides to illustrate this. In the first few days after birth, gap
junctions (the space in between cells) are open and "leaky" allowing for
substances to easily cross into milk from the bloodstream. That is not really a
big deal since the babies are getting a very small amount of colostrum.
Any medication that mom takes is not likely to have much of an effect because
the baby is not taking in (appropriately!) a large amount of colostrum.
<---
I have cool
slides to illustrate this. In the first few days after birth, gap
junctions (the space in between cells) are open and "leaky" allowing for
substances to easily cross into milk from the bloodstream. That is not really a
big deal since the babies are getting a very small amount of colostrum.
Any medication that mom takes is not likely to have much of an effect because
the baby is not taking in (appropriately!) a large amount of colostrum.
By about day 4 of life, those gap junctions close, meaning any medication now would need to penetrate 2 lipid bilayers to get into milk. After closure of the gap junctions, a medication would need to have certain characteristics or transporters to get into milk. For example, molecules that easily get into milk need to be small and lipophilic (meaning the molecule can interact easily with lipids). Substances like alcohol are in this lipophilic category. Because they are lipophilic, they can go right through the blood:milk barrier, but then come right out (illustrated the "simple diffusion" slide) . Other molecules have specialized transporters so they can enter milk. Others, like secretory IgA, have a special protein transporter. I have illustrated all these ideas in the "cool slides."
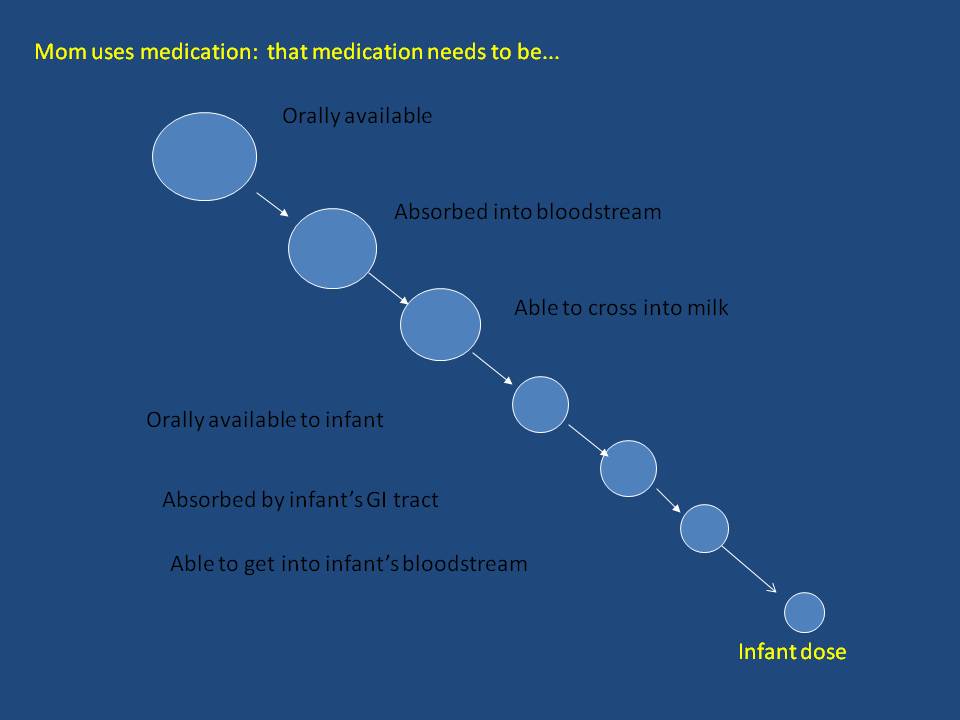
For a drug to make a difference:
It
needs to be orally available: That means that if the baby gets the medication from drinking breastmilk, the medication needs to work if taken orally. Many medications don't work orally. For example, Heparin, Aminoglycosides and third generation cephalosporins (the last two are classes of antibiotics), and radiocontrast agents (for MRI or CT scans) do not work if taken orally. Often they are injections or given IV. If you gave those medications orally, they would have little effect. So, if the baby would get the medication by drinking breastmilk, it makes little difference. That's not how that medication works.I
t needs to absorbed through the GI tract: The medication only has an effect if it can get into the maternal bloodstream. If it can't be absorbed from the GI tract into the bloodstream, it can not get into milk. Examples of medications that are into absorbed from the GI tract and can not get into the bloodstream in significant amounts are morphine and sumatriptan (which are sequestered in the liver), gadolinium salts (used in MRIs), iodinated contrast agents (used for CTs) and Vancomycin (an antibiotic). Take note here: MRIs and CT scans can be done safely without discarding milk.•Transferred into milk: Large molecular weight proteins like insulin and interferon can not cross the very protective blood:milk barrier because they are too big to get through those lipid bilayers and therefore they do not cross into breastmilk.
•Orally available to infant: Could the baby ingest it and have it do something clinically? If the medication is not given in a way that is meant to work by taking it by mouth it is unlikely to have an effect on the baby. For example, intravenous medications aren't ingested, so they make little difference. Topical medications aren't eaten so they are considered compatible with breastfeeding.
•Absorbed by infant GI tract. Can the baby digest it? A topical medication wouldn't be eaten, nor digested. Therefore, they don't get into the bloodstream and make excellent medication choices if possible.
•Present in a clinically significant amount: When it finally makes into the babies bloodstream, if it does, how much gets there?
I
f the medication cannot get into the bloodstream, it cannot get into the breastmilk.We need to consider:
•Amount transferred to the infant: After all the considerations we have talked about, what gets to the baby is likely to be less than what mom originally took. An exception to that would be alcohol; the amount of alcohol in mom's blood is exactly that in her milk. (Remember, alcohol is lipophilic, small in size, gets into the maternal bloodstream, is orally available to the baby and can be digested by the baby-- pretty much everything that makes a substance able to enter breastmilk.)
•The age of the infant: The amount that a 10 month old, who is taking solids, weighs double or nearly triple their birth weight, and is probably nursing less frequently, will be very different that the amount that an infant receives.
•Effects of the medication on the baby: Some of the same side effects that mom experiences may occur in the baby. While antibiotics are almost all compatible with breastfeeding, the amount that crosses into milk can cause diarrhea or yeast infections in the baby.
•Effects
of the medication on maternal milk supply: Let's not forget this one! A
medication may be perfectly compatible with breastfeeding for mother and
baby but works on a hormone that makes milk. For example,
bupropion (otherwise known as Wellbutrin and Zyban)
is compatible with breastfeeding but increases dopamine. Dopamine decreases
prolactin, the hormone that makes milk. So when this medication increases
dopamine, it decreases prolactin, which can then decrease the amount of milk
produced.
Points to remember:
Breastfeeding is important! When we do a risk:benefit analysis for the medication, we need to consider the risks of not breastfeeding. "Just to be safe" overwhelmingly means continuing to breastfeed.
The
information is out there. Anyone can access it. Sometimes synthesizing all
that information requires some help. And help is out there. Please tell me you
will find it.
It’s
better to assume that the medication is compatible (not safe) than
ask the mother to pump and discard her milk without researching the answer.
What medication can I take
while I'm breastfeeding?
General Guidelines:
-
We don't throw milk away without a really, really good reason. Like you are getting chemotherapy or decided to do heroin.
-
Most medications are compatible (I try to avoid saying "safe") with breastfeeding.
-
If you don't really need to take it (like cold medications) don't take it.
Resources:
-
LactMed: This is the resource recommended by the American Academy of Pediatrics. Try it right now if you'd like. Your inquiry will go to the National Library of Medicine page dedicated to medications in breastmilk. They also have an app that you can download right to your phone so that you always have access to the information you need and can share if you need to. (I have asked mothers to download it right in my office if I know they are having a procedure, surgery or are having medical problems. They can share that information with their providers right on the spot.)
- and Me, although I'm just going to check LactMed
back to www.drjen4kids.com